Quick summary
Coordinating insurance coverage after a job change is about three things: timing, choices, and costs. First, identify when your old coverage ends and when new benefits begin. Second, evaluate bridging options (COBRA, Marketplace special enrollment, short‑term plans). Third, update beneficiaries and consider private alternatives for life or disability coverage that aren’t portable.
This guide gives a step‑by‑step timeline, real‑world tradeoffs, and specific paperwork and deadlines to watch — based on current U.S. rules from the Department of Labor and HealthCare.gov and my 15 years advising clients through job transitions.
Step‑by‑step timeline for a smooth transition
- Immediately (before you leave or the day you give notice)
- Ask current HR: what is your exact coverage end date? Is it the last day of employment or the end of the month?
- Ask incoming HR: when does employer coverage start? Is there an eligibility waiting period (commonly 0–90 days)? Get these dates in writing.
- Request copies of plan summaries and the COBRA notice you’re entitled to receive on exit.
- Within 7 days after separation
- Read the COBRA election materials carefully. Federal rules give you a 60‑day window to elect COBRA continuation coverage starting from the date you receive the election notice or the date coverage ended (whichever is later) — see Department of Labor guidance (DOL) for details.[1]
- Confirm whether a Special Enrollment Period (SEP) for the Health Insurance Marketplace applies. If you lose job‑based coverage, you typically have 60 days to enroll in a Marketplace plan.[2]
- Before coverage gap occurs
- If the new employer plan starts after your old coverage ends, choose one bridging option: elect COBRA, enroll in a Marketplace plan during the SEP, or buy a short‑term plan if appropriate (short‑term plans are generally cheaper but are not ACA‑compliant and can exclude pre‑existing conditions).[2]
- Compare total monthly cost and expected out‑of‑pocket costs, not just premiums. COBRA generally allows you to keep the exact same plan but you will pay the full premium (up to 102% of the plan cost, which can be expensive).[1]
- After new coverage begins
- Confirm the new plan’s start date and verify coverage (e.g., login to insurer portal, check ID card). If you enrolled in COBRA and later become eligible for employer coverage, you can terminate COBRA coverage when the new plan is active.
- Update providers if needed and transfer medical records or prescriptions to in‑network providers.
Health insurance: key options and pros/cons
-
COBRA continuation coverage
-
Pros: Keeps your exact employer plan and network; preserves preexisting condition protections in the same plan.
-
Cons: You pay the full premium plus administrative fee (up to 102%); typically available for up to 18 months for involuntary termination or 36 months for other qualifying events — check DOL rules.[1]
-
Action: Don’t miss the 60‑day election window and note that coverage is retroactive to your loss date if you elect COBRA and pay back premiums.
-
Health Insurance Marketplace (ACA) plans
-
Pros: Often more affordable than COBRA (especially with subsidies), comprehensive coverage, protections for preexisting conditions.
-
Cons: Plan networks and formularies differ from employer plans; comparing expected total costs takes work.
-
Action: Check if you qualify for premium tax credits using HealthCare.gov and enroll during the Marketplace SEP (typically up to 60 days from loss of coverage).[2]
-
Short‑term health plans
-
Pros: Lower premiums for short gaps, quick start dates.
-
Cons: Not ACA compliant — may exclude preexisting conditions, limit benefits, or have lifetime limits. Use only as a deliberate bridge and read exclusions carefully.[3]
-
Action: See our explanation of when short‑term plans make sense: “When to Use Short‑Term Health Insurance and What It Covers”.
(Internal resources: What is COBRA continuation coverage?, When to Use Short‑Term Health Insurance and What It Covers, Coordinating Health Coverage After Job Loss.)
Life and disability insurance: portability and replacement
- Group life insurance through an employer is usually term coverage and often not portable. Some policies include a conversion or portability option (at higher cost); others end on your last day. Check the group policy document for conversion rights and timelines.
- Employer short‑term and long‑term disability policies typically end when employment ends. If the new employer’s plan is weaker or has a waiting period, consider buying an individual disability policy to avoid gaps in wage replacement protection.
- Action: Immediately update beneficiary designations on retirement and life accounts and request a copy of the group policy’s conversion rules. Contact a licensed agent to price individual life and disability alternatives if portability is not available.
Account‑based benefits: HSAs, FSAs, and dependent coverage
- HSA (Health Savings Account)
- If you were contributing to an HSA linked to a high‑deductible health plan (HDHP), you remain the account owner after leaving the job. You can continue to use the funds tax‑free for qualified medical expenses but you can’t make new HSA contributions unless you’re covered by an HSA‑eligible HDHP. See IRS Publication 969 for HSA rules.[4]
- FSA (Flexible Spending Account)
- Employer FSAs often have a plan year and run‑out period. In some limited cases you may be able to elect COBRA for a health FSA balance depending on plan design — confirm with HR and plan documents.
- Dependent coverage and COBRA
- Dependents (spouse, children) usually qualify for COBRA as well; election windows and maximum coverage lengths may differ.
Practical examples and cost tradeoffs
- Example 1 – Short waiting period gap: If your new employer’s plan starts 30 days after your last day and COBRA premium is $1,200/month vs. a Marketplace plan at $450/month after subsidy, the Marketplace option could save several hundred dollars. But if you expect high medical costs and value the old plan’s network and drug formulary, COBRA may be worth the price.
- Example 2 – Immediate new plan but you want to keep HSA eligibility: If the new plan isn’t HSA‑eligible, you can’t make new HSA contributions — consider timing contributions or using catch‑up contributions if eligible.
In my practice I’ve helped clients avoid unnecessary COBRA costs by verifying immediate eligibility at their new employer (sometimes HR processes allow retroactive enrollment). Always confirm dates in writing before electing expensive continuation coverage.
Common mistakes to avoid
- Assuming employer coverage continues automatically after your last paycheck — always confirm the exact end date.
- Forgetting the 60‑day COBRA election and Marketplace SEP windows.
- Choosing a short‑term plan without checking exclusions and prescription drug coverage.
- Losing track of beneficiary updates when changing jobs.
Action checklist before and after a job change
- Before leaving: get coverage end date and new plan effective date in writing.
- Within a week of separation: gather COBRA materials and confirm SEP deadlines for Marketplace enrollment.[1][2]
- Compare costs: COBRA full premium vs. Marketplace vs. short‑term plan (include deductibles, networks, and expected spending).
- Update beneficiaries for life and retirement plans and evaluate portability/conversion options for group life insurance.
- If you have an HSA, track contribution limits and eligibility; roll over FSA balances if allowed by your plan.
- After new coverage begins: verify ID cards, provider network, and prescription coverage; terminate any overlapping temporary coverage.
Sources and further reading
- Department of Labor — COBRA questions and answers: https://www.dol.gov/agencies/ebsa/about-ebsa/our-activities/resource-center/faqs/cobra-continuation-health-coverage [1]
- HealthCare.gov — Special Enrollment Periods and buying coverage after losing job‑based insurance: https://www.healthcare.gov/coverage-outside-open-enrollment/special-enrollment-period/ [2]
- HealthCare.gov — Short‑term limited duration insurance explanation: https://www.healthcare.gov/coverage-outside-open-enrollment/short-term-plans/ [3]
- IRS Publication 969 — Health Savings Accounts and other tax‑favored health plans: https://www.irs.gov/pub/irs-pdf/p969.pdf [4]
Professional disclaimer
This article is educational and general in nature and does not constitute personalized legal, tax, or insurance advice. Rules and plan terms change; confirm specific deadlines, costs, and conversion rights with your employer’s benefits administrator and insurers. For tailored advice, consult a licensed insurance agent or a financial planner.
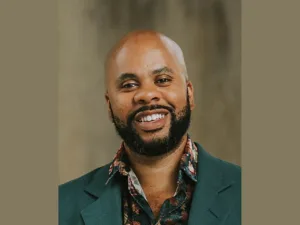
Author note: In my 15 years helping people navigate job transitions, the single most effective step is early communication with both employers’ HR teams — it reduces surprises and often uncovers cheaper or faster solutions than initially apparent.