Introduction
Starting a family changes how you should think about health insurance. You’re not just buying coverage for routine care — you’re budgeting for prenatal visits, delivery, neonatal care, and frequent pediatric appointments. The right plan minimizes surprise bills and protects your household cash flow during one of life’s most important transitions.
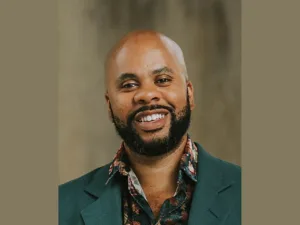
In my 15+ years advising families, I’ve seen two patterns: people either focus only on the monthly premium and get surprised by high out-of-pocket costs, or they over-insure and pay more than necessary. This guide lays out the practical steps to choose a plan that fits medical needs and financial goals.
Sources referenced in this article include HealthCare.gov, the Centers for Medicare & Medicaid Services (CMS), and state Medicaid resources (see Sources section for links). This is educational content and not personalized advice—consult your benefits administrator or insurance broker for plan-specific guidance.
Compare the core plan features that matter most
When assessing plans, compare these features side-by-side for a one-year total-cost view:
- Premium: monthly cost to keep a policy active. Cheap premiums can be tempting but may signal higher cost-sharing elsewhere.
- Deductible: the amount you pay before most benefits kick in. A high deductible plan raises your up-front risk if pregnancy or newborn care is needed.
- Coinsurance and copays: how much you pay after hitting the deductible (e.g., 20% coinsurance or $40 per visit).
- Out-of-pocket maximum (OOPM): the safety cap on how much you will pay in a year. For new families, a lower OOPM can be the single most important protection.
- Provider network: whether your chosen hospital, OB/GYN, and pediatricians are in-network (in-network care is far cheaper).
- Coverage specifics: maternity care, labor and delivery, neonatal intensive care (NICU), well-child visits, vaccines, and lactation support.
For side-by-side comparison tools, HealthCare.gov provides plan details and estimated costs by county/state (https://www.healthcare.gov/).
Practical tip: run a “total cost” scenario
Estimate expected costs for the year: add 12 months of premiums plus expected out-of-pocket spending (deductible, copays, coinsurance) for prenatal care, delivery, and the newborn’s first-year routine care. Compare totals across plans rather than picking the lowest premium alone.
Plan types and how they usually fit new families
- Employer-Sponsored Insurance (ESI): Often has lower employer-subsidized premiums and coordinated benefits. Check whether your employer’s plan includes approved maternity care providers and whether you can add a dependent mid-year for birth.
- Marketplace (ACA) plans: Eligible families may qualify for premium tax credits (Advanced Premium Tax Credit, APTC) and cost-sharing reductions if income falls within program limits. Marketplace plans must cover maternity and newborn care as essential health benefits (HealthCare.gov).
- Medicaid and CHIP: For eligible low-income parents and infants, Medicaid and the Children’s Health Insurance Program (CHIP) provide comprehensive maternity and pediatric coverage with low or no cost-sharing. Eligibility is state-dependent (https://www.medicaid.gov/).
- Short-term/gap plans: Generally not recommended for expectant families because many exclude maternity and pre-existing conditions.
Networks: pick providers first, plans second
Networks matter more when starting a family than for many other life stages. Verify:
- Your preferred OB/GYN and hospital (and their neonatology team) are in-network.
- Local pediatricians you prefer accept the plan.
- If you have a planned delivery location, confirm facility network status — some hospitals have out-of-network billing practices that can lead to large surprise bills.
For more on how networks affect bills and how to check them, see our related piece: How Health Insurance Networks Affect Your Medical Bills.
Maternity, newborn, and pediatric coverage specifics to review
- Prenatal care: number of covered prenatal visits and whether screening tests are included.
- Labor and delivery: inpatient facility coverage, anesthesia, and delivery complications (e.g., C-section coverage).
- NICU and newborn complications: check coinsurance for neonatal intensive care — NICU stays can be very expensive.
- Postpartum care and mental health: coverage for postpartum follow-up and behavioral health services.
- Well-child visits and immunizations: many plans cover these at no additional cost under ACA rules.
Money math: estimating total one-year cost (an example)
Example family scenario:
- Plan A: Premium $400/mo = $4,800 yearly; deductible $2,000; OOPM $6,000.
- Plan B: Premium $550/mo = $6,600 yearly; deductible $500; OOPM $3,000.
If the pregnancy and delivery generate $8,000 in covered charges:
- Plan A out-of-pocket: pay deductible $2,000 + coinsurance until OOPM; assume final OOP ~ $6,000 plus premiums = $10,800 total.
- Plan B out-of-pocket: deductible $500 + coinsurance to OOPM $3,000 plus premiums = $9,600 total.
Although Plan B has higher premiums, the lower deductible and OOPM produced a smaller total cost for the year. Run similar calculations with realistic cost assumptions for your area and provider network.
For more on how deductibles affect your budget, see: How Health Insurance Deductibles Affect Your Budget.
Enrollment timing and special enrollment periods (SEPs)
- Annual open enrollment windows apply for Marketplace plans; employer plans also have annual enrollment periods.
- Birth of a child is a qualifying life event that triggers a Special Enrollment Period (SEP). You generally have 60 days to add a newborn to your plan or switch plans after a birth.
- Pregnancy itself is not always a qualifying event for plan changes before birth, but some states and employers allow mid-year changes for pregnancy—check plan rules and state resources (HealthCare.gov).
Financial help and tax credits
- Premium Tax Credits (APTC): If you buy through the ACA Marketplace and your household income is within set limits, you may qualify for subsidies that lower monthly premiums. Reconcile any APTC amounts when you file taxes.
- Cost Sharing Reductions (CSR): Available with certain Marketplace silver plans if you qualify by income; they lower deductibles and coinsurance.
- Medicaid/CHIP: For eligible families, these programs can reduce or eliminate out-of-pocket costs for maternity and pediatric care. Use your state’s Medicaid website to confirm eligibility and benefits.
Self-employed or small-business considerations
Self-employed parents may qualify to deduct health insurance premiums on their tax return (see IRS guidance and Form 1040 instructions). If you purchase Marketplace coverage, be sure to understand how APTC reconciliation on Form 8962 works when filing taxes. For employer-offered small-business credits and forms like Form 8941, consult a tax professional or the IRS site (IRS.gov).
Practical checklist before you enroll
- Confirm provider network for OB/GYN, hospital, neonatology, and preferred pediatricians.
- Compare one-year total cost (12x premiums + estimated out-of-pocket medical costs).
- Check maternity, NICU, and postpartum mental health coverage specifics.
- Verify newborn enrollment timeline and SEP rules in your plan.
- If buying on the Marketplace, estimate APTC and whether a silver plan with CSR is advantageous.
- Build or adjust your emergency fund to cover at least your chosen plan’s deductible plus 1–2 months of premiums (see our guide: Coordinating Health Insurance with Emergency Savings).
Common mistakes new parents make
- Choosing solely on lowest premium without modeling total costs.
- Failing to check whether the delivery hospital or OB is in-network.
- Missing the SEP timeline to add a newborn or change plans after birth.
- Assuming short-term plans cover maternity or pre-existing conditions — they usually do not.
Quick FAQ
- Can I enroll in Medicaid during pregnancy? Yes — many states have enhanced Medicaid eligibility for pregnant people; apply through your state Medicaid office (https://www.medicaid.gov/).
- Does Marketplace coverage have to include maternity care? Yes, maternity and newborn care are essential health benefits required in ACA-compliant plans (HealthCare.gov).
- If I’m covered under my partner’s plan, when should I switch? Evaluate cost and network coverage early in pregnancy; switching can be done at open enrollment or after the birth SEP.
Sources and further reading
- HealthCare.gov — Maternity and newborn care; Marketplaces and SEPs: https://www.healthcare.gov/
- Medicaid.gov — State-by-state Medicaid and CHIP information: https://www.medicaid.gov/
- IRS — Affordable Care Act information and tax forms: https://www.irs.gov/affordable-care-act
- CMS — Regulatory guidance and consumer information: https://www.cms.gov/
Professional disclaimer
This article is educational and does not replace personalized advice from an insurance broker, benefits administrator, or tax professional. In my practice, I recommend running realistic cost scenarios and speaking with your providers to confirm network status before finalizing coverage.
If you’d like help estimating total one-year costs for a specific plan, prepare your premium, deductible, coinsurance rates, and a list of anticipated services; a financial advisor or benefits counselor can run the numbers with you.